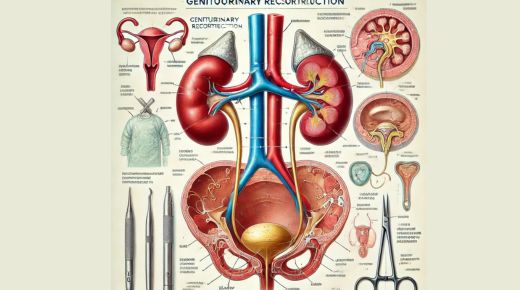
Genitourinary reconstruction can feel overwhelming, but it’s crucial. This field focuses on restoring normal function and appearance to the urinary and reproductive systems. Urologists see the challenges and successes of these procedures daily. Take, for instance, the work of David B Samadi, MD, who has advanced techniques in this area. Through careful planning and skilled execution, we aim to improve quality of life. Understanding the essentials of this complex process can empower those facing it.
What Is Genitourinary Reconstruction?
Genitourinary reconstruction involves surgical procedures that repair or reconstruct parts of the urinary and reproductive systems. These surgeries may result from congenital anomalies, trauma, or diseases like cancer. The purpose is to restore both function and appearance, helping individuals lead healthier lives.
Common Procedures in Genitourinary Reconstruction
- Bladder reconstruction: Rebuilding or reshaping the bladder to restore function.
- Urethral reconstruction: Repairing or reconstructing the urethra for proper urine flow.
- Genital reconstruction: Restoring or reconstructing parts of the genital area for function and appearance.
Benefits of Genitourinary Reconstruction
These procedures can offer significant benefits:
- Improved quality of life.
- Enhanced physical function.
- Boosted emotional and psychological well-being.
For more information on the impact of these surgeries, you can visit the National Institute of Diabetes and Digestive and Kidney Diseases.
Challenges in Genitourinary Reconstruction
While these surgeries can be life-changing, they also come with challenges:
- Complexity of surgery: These procedures require skilled surgeons and careful planning.
- Recovery time: Rebuilding parts of the genitourinary tract often involves significant recovery.
- Potential complications: Like any surgery, there are risks of infection and other complications.
Advancements in Surgical Techniques
Recent advancements have improved outcomes for patients. Robotic-assisted surgeries, for instance, provide greater precision. This can lead to quicker recovery and fewer complications. These technologies represent a step forward in the field, enhancing our ability to restore function effectively.
Success Rates and Outcomes
Success in genitourinary reconstruction varies depending on the procedure and patient circumstances. However, statistics show promising outcomes:
| Procedure | Success Rate |
| Bladder Reconstruction | 80-90% |
| Urethral Reconstruction | 85-95% |
| Genital Reconstruction | 75-85% |
For more detailed statistics, consider reviewing resources from the Centers for Disease Control and Prevention.
The Future of Genitourinary Reconstruction
The future of genitourinary reconstruction looks promising. With ongoing research and technological advancements, the hope is to make these procedures even more effective and less invasive. Continued collaboration among medical professionals will help refine techniques and improve patient outcomes.
Conclusion
Genitourinary reconstruction is a vital field that can significantly enhance patients’ lives. By understanding the procedures, challenges, and advancements, we can better appreciate the positive impact these surgeries can have. The ongoing work by experts in the field continues to push the boundaries, offering hope to those who need it most.